This vascular condition, which can result in the arteries to the legs and feet becoming narrowed or blocked, affects one out of five adults over the age of 55 in the United States.
Danielle Bajakian, MD, Director of the Critical Limb Ischemia Program at the Division of Vascular Surgery and Endovascular Interventions, explains that PAD is significantly underdiagnosed, despite a steady increase in prevalence due to rising rates of obesity and diabetes. If you or a loved one has any of the risk factors for PAD, here is what you need to know.
What causes PAD?
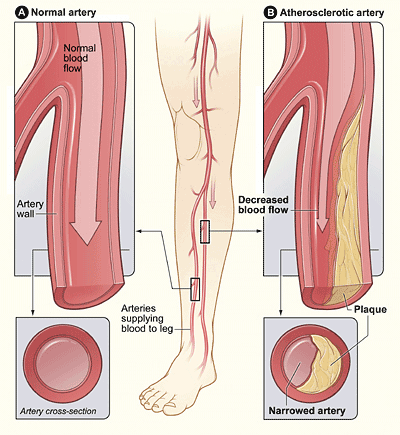
PAD is caused by the buildup of fatty deposits or plaques in the arteries leading to the legs.
Why is PAD a serious problem?
If the arteries become too narrowed, the extremities may not receive enough oxygen to function properly. The most common symptom is debilitating pain or cramping after walking (claudication). More severe symptoms include pain in the foot or calf at rest without walking or wounds in the toes or foot that does not heal. Other symptoms may include numbness or weakness of the leg, change in the color of the skin. In the most severe form of the disease, the toes or foot may become gangrenous (called critical limb ischemia, or CLI), and the limb may need to be amputated.
In addition to its risk to the legs, PAD also affects other organs in the body, including the heart and brain. People with PAD have a 40% increased risk of having a heart attack and stroke because blood flow to the heart and brain may be restricted. In short, a diagnosis of PAD should be considered a wakeup call to take control over one’s health.
What are the risk factors for PAD?
The main risk factors for PAD include diabetes, smoking, obesity, advanced age, high cholesterol, and high blood pressure. Family history of PAD also increases a person’s risk. “We can modify two of these important factors – obesity and smoking,” says Dr. Bajakian. Taking steps to maintain a healthy weight can also improve type 2 diabetes, blood pressure, and cholesterol levels in the process.
What can one do to prevent critical limb ischemia?
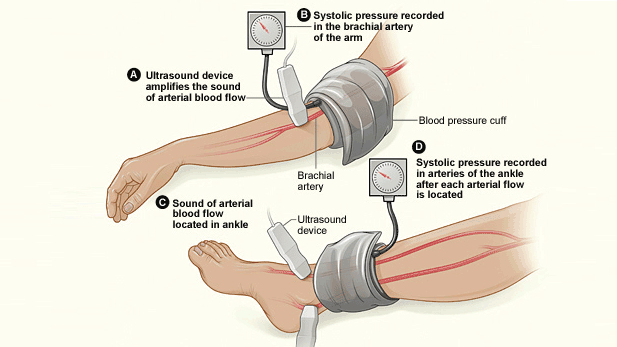
Dr. Bajakian says the importance of early evaluation cannot be overstated: if a person has risk factors for PAD, and especially if there are any symptoms such as leg pain or wounds that don’t heal, he or she should see a vascular specialist. Initial evaluation can be done through a simple, noninvasive test called ankle brachial index, which compares the blood pressure in the arm to the blood pressure in the leg. This quickly reveals whether the circulation in the legs is abnormal and should lead to further evaluation by a vascular specialist. Some primary care providers now perform ankle brachial index testing in their offices.
According to Dr. Bajakian, “Early diagnosis and care is very important because it could save you from having a heart attack or stroke. There can be devastating consequences if you are diagnosed with advanced disease. But there is no harm in coming in early for evaluation if you believe you have even mild symptoms.”
About half of patients with PAD can be treated with lifestyle changes, exercise, and medications alone. The single most important thing a person can do to reduce complications from vascular disease is to quit smoking. For patients with diabetes, maintaining good control of blood sugar is critical. Dr. Bajakian warns that patients who have diabetes and smoke are at the highest risk of all, as they develop vascular disease at an accelerated rate compared to other patients.
How is PAD/CLI treated?
In addition to optimal management of diabetes and smoking cessation, treatment of PAD includes medications to control blood pressure and cholesterol, prevent blood clots, and to treat pain.
If these are insufficient, interventional treatments include endovascular procedures and traditional bypass operations. The most common endovascular procedure, angioplasty, is a procedure in which a catheter is threaded through an incision in the groin into the narrowed artery. A small balloon on the tip of the catheter is deployed to flatten the fatty deposits, widen the artery, and restore blood flow through the area. In some cases, a stent, or wire mesh, is placed to keep the artery open. Another option is known as atherectomy, in which a catheter is advanced into the narrowed vessel and the surgeon removes the plaque from the inside of the artery.
Endovascular procedures treat narrowed arteries with virtually no recovery period. Until fairly recently, results after endovascular procedures were not long lasting, and many patients required frequent procedures to treat their symptoms. After such procedures, restenosis, or scarring of the tissue inside the artery, would gradually cause the artery to narrow again. About 40% of patients would need to return for second procedures each year. However since 2014, medications to prevent the formation of scar tissue have been added to the stents and balloons. Studies of drug-coated devices show that results are significantly improved compared to angioplasty or stenting alone. “Data is early, but it looks very promising. We are hopeful that patients will not have to return for reoperation,” says Dr. Bajakian. “With the drug coated stents and balloons, fewer than 10% of patients have recurrent symptoms each year.”
About 80% of patients at NYP/Columbia’s Division of Vascular Surgery and Endovascular Interventions who require intervention to open blocked arteries are able to have minimally invasive endovascular procedures, but some patients still require traditional bypass operations. During bypass procedures, the surgeon creates a new route for the blood to flow, either by using a blood vessel from another part of the body, or by placing a synthetic graft. The advantage of bypass procedures is that the results last a long time, with most patients not needing to return for reoperation. In comparison to endovascular procedures, however, bypass grafting is followed by a longer recovery time. As Dr. Bajakian explains, “Bypass operations can be extremely beneficial in patients who have failed endovascular procedures.”
At NYP/Columbia, the Critical Limb Ischemia program works closely with podiatrists, endocrinologists, cardiologists, internists, and other specialists to evaluate and treat patients as early as possible.
Dr. Bajakian and her colleagues have studied many of the endovascular devices and medications now in use. Other approaches on the horizon include attempts to grow new blood vessels (angiogenesis) by injecting medications that promote the growth of blood vessels along the blocked artery. In addition to a new angiogenesis drug trial now underway, NYP/Columbia will soon begin a pivotal trial of a new drug coated stent, with Dr. Bajakian as the Principal Investigator.