For decades, patients with failing kidneys have been sustained by hemodialysis, or dialysis for short – the process of removing the blood from the body, filtering it through a machine, and returning it back to the body. Today dialysis is a life-saving option for over 600,000 people in the U.S., usually in the form of several treatments per week. That number of patients is growing due the rising incidence of diabetes, which can cause kidney failure, as well as other factors such as the use of medications that contribute to kidney failure. No matter the cause of kidney failure, every dialysis patient must have what is called vascular access. As the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) describes it, vascular access is so important that it can be considered ‘a hemodialysis patient’s lifeline.’ This is a specially prepared entry point where the dialysis needle will be inserted during every treatment; without it, dialysis cannot be performed.
There are three primary types of vascular access, each with its advantages and disadvantages.
AV fistula
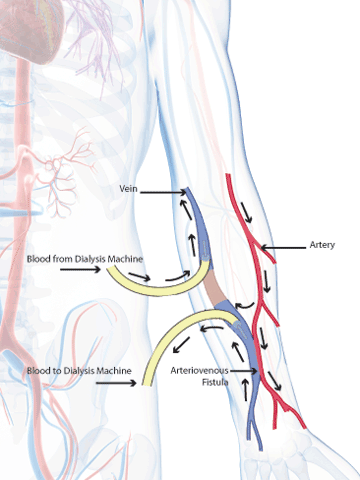
Arteriovenous (AV) fistula is the connection of an artery to a vein, usually in the forearm. Creating this connection causes extra blood to flow through the vein, which makes it grow larger and stronger. This allows for repeated use during dialysis. Untreated veins cannot be used for repeated dialysis because they would collapse. AV fistulas are considered the most ideal type of vascular access because they provide good blood flow, they are the least likely type to become infected or cause clots, and they last the longest.
After surgery to create an AV fistula, it is not immediately ready for use: the fistula must ‘mature.’ This process, in which the vein grows larger and thicker, may take two to three months.
AV graft
An arteriovenous graft is similar to that of an AV fistula, but instead of connecting the patient’s artery to vein, a teflon tube is used to connect these vessels. An AV graft may be used if the patient’s blood vessels are too small or clotted to create an AV fistula. AV grafts mature more quickly than fistulas (two to three weeks, rather than months), but they are more prone to infection and clotting, and are therefore used far less commonly.
Venous catheter
A venous catheter is a thin tube inserted into a vein in the neck, chest, or groin. Venous catheters can be used for dialysis right away, which is important if a patient has a sudden kidney problem and cannot wait for a fistula or graft to mature. Venous catheters are the most likely of all three types to be compromised by infection and clotting, and are therefore used only for short-term dialysis.
Dialysis access procedures are performed by vascular surgeons such as Dr. Nicholas J. Morrissey, Associate Professor of Surgery and Bicampus Director of Clinical Trials for the Division of Vascular Surgery. Dr. Morrissey performs about 90% of dialysis access procedures at NewYork-Presbyterian/Columbia’s Department of Surgery.
Once the AV fistula or graft is in place, his job is far from done: ongoing maintenance of the access is crucial to the patient’s long-term health and well-being. Narrowing of the vascular access is common, most often due to the formation of scar tissue. Infection and clotting are also fairly common complications. For a patient whose life depends on regular cleansing of the blood, the last thing he or she needs is to arrive for treatment and find his or her lifeline obstructed. “Dialysis access points need to be continually and carefully monitored. If the vessels show narrowing, they may need to be reopened with an angiogram or stent,” explains Dr. Morrissey. If an access fails, the patient may have to have a new one created.
As with most things in life, prevention is worth its weight in gold. Patients can help to avoid access failure by being vigilant about any signs of infection, reduced blood flow, or other problems.
Access failure can be prevented through steps including
- Not allowing anyone to draw blood from the arm where the access is located
- Have kidney function assessed routinely
- At every dialysis session, check to see if dialysis is proceeding efficiently or if blood is not clearing well.
- Note any prolonged bleeding after removal of the needle; excessive bleeding could indicate high pressure that could indicate failure.
- If there are signs of high pressure, or if the alarm goes off during dialysis (indicating a possible blockage), patients should seek evaluation of their access immediately.
“If we can identify and preserve good veins, a person can get through his or her entire life with one access,” says Dr. Morrissey.
As the need for dialysis continues to grow, Dr. Morrissey is on the forefront of research in developing improved surgical techniques, as well as identifying the best practices for preserving and maintaining a patient’s access. Later this year, he will direct a trial of an endovascular approach to creating AV fistula; this minimally invasive method allows surgeons to create the access through a catheter, using angiography rather than open surgery. Although this approach has been in use outside the U.S., this upcoming trial will represent its debut here in the States.
Dr. Morrissey is also coordinating research that will track patients long term and help to identify factors that predict access failure, so that surgeons can intervene before failure occurs.
The Division of Vascular Surgery and Endovascular Interventions works very closely with specialists in nephrology, diabetes, and others at NYP/Columbia to ensure that patients who need vascular access receive prompt and seamless care.
