Story By Julia Chang; Video By Emily Driscoll, Katie Garrett and Rick Brown
In a sunny playroom on the sixth floor of NewYork-Presbyterian Morgan Stanley Children’s Hospital, two baby girls, clad in pink and wearing white headbands, pose for a photo together in their mothers’ arms, although they spend more time looking curiously at each other than at the camera.
Mia Skaats, 8 months old, and Brooklyn Civil, 2 months old, were strangers before today, but in some ways their meeting feels like a reunion. Both were born with rare, life-threatening congenital heart defects. Both had spent much of their short lives in the hospital’s neonatal cardiac intensive care unit (NCICU). And less than two weeks prior, both were part of the first-ever domino heart valve transplant in infants — an unprecedented procedure that involved transplanting parts of Mia’s heart into Brooklyn’s.
A domino transplant happens when one patient receives an organ transplant and, in turn, donates a healthy organ or healthy parts of an organ to another patient, becoming both a recipient and a live donor. In Mia and Brooklyn’s case, Mia received a full heart transplant, which then made it possible for the healthy valves from her old heart to be placed into Brooklyn’s heart through a partial heart transplant. Making it all happen required the right patients, the right timing, and the tireless teamwork of a multidisciplinary care team that included the transplant service team, child life services, nurses, doctors, the perioperative and surgical teams, and more.
“To me, the biggest part of this is that we went from helping one baby to two,” says Dr. Marc Richmond, a pediatric cardiologist and director of the Program for Pediatric Cardiomyopathy, Heart Failure and Transplantation at Columbia/NewYork-Presbyterian Morgan Stanley Children’s Hospital, who led the girls’ pre- and postoperative medical care teams. “The No. 1 reason babies die while on a transplant list is because they don’t match with a donor fast enough. So the ability to help more than one child — that’s the holy grail for us. There were dozens of people in the hospital caring directly for both children. It was a whole team effort.”

‘The Timing Was Very Serendipitous’
The idea that Mia and Brooklyn could be the right candidates for a domino heart valve transplant began to come together the morning of Wednesday, May 10, 2023, around 7 a.m., when the pediatric cardiology and surgical teams met to go over their patient case list.
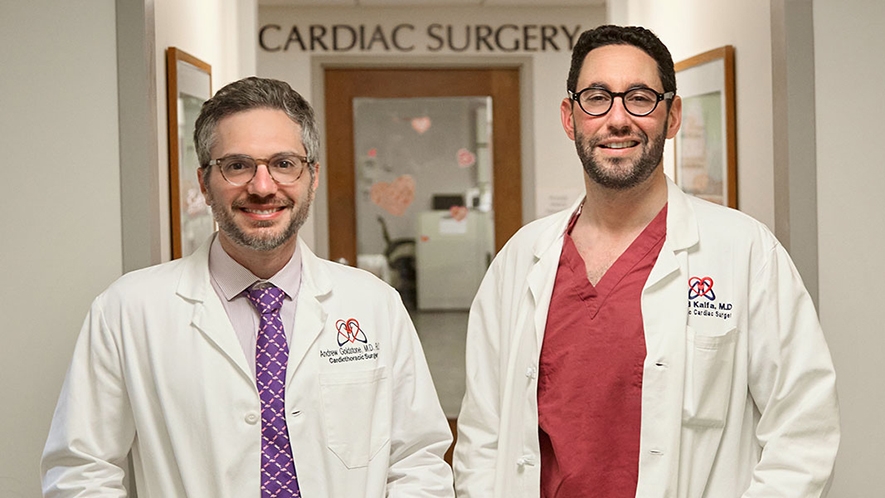
Dr. Andrew Goldstone, pediatric heart surgeon at Columbia/NewYork-Presbyterian Morgan Stanley Children’s Hospital, was the on-call transplant surgeon that day. He had accepted a donor heart overnight for Mia, who had a form of cardiomyopathy that causes a thickening and weakening of the heart muscle, which made it difficult for her heart to squeeze and pump blood to her body. Mia was in heart failure and had been in the NCICU for seven months waiting for a donor. Her transplant was scheduled for later that day.
When the team began discussing Brooklyn’s case, the pieces started to come together. Brooklyn had been diagnosed at her mother’s 20-week prenatal ultrasound with truncus arteriosus, a rare condition in which her heart never developed a pulmonary valve and aortic valve, the two valves needed to pump blood out from the heart. Instead, she was born with a single outflow valve, known as a truncal valve, and a hole between the two pumping chambers of her heart.
Dr. David Kalfa, pediatric heart surgeon at Columbia/NewYork-Presbyterian Morgan Stanley Children’s Hospital, had performed surgery on Brooklyn when she was 4 days old to help treat her condition because she had severe leakage and obstruction of her truncal valve. He repaired the hole in her heart, connected her pulmonary artery directly to her right ventricle to allow blood flow to her lungs, and used her truncal valve as an aortic valve to pump blood to the rest of her body. But the surgery wasn’t meant to be a long-term solution as her truncal valve was leaky, which meant blood was flowing backward into her heart and causing it to enlarge and become weaker. Unless her valve could be replaced, Brooklyn’s heart would fail.
Brooklyn’s existing options weren’t ideal. Tissue valves from a pig or a cow or cryopreserved valves from a deceased human donor tend to wear out quickly in babies. Mechanical valves carry a high risk for blood clots and thus require lifelong use of blood thinners — plus, they typically aren’t small enough to fit a tiny infant’s heart. And none of these would have grown with Brooklyn as she grows, which meant she’d need multiple surgeries during childhood. Dr. Kalfa knew her best option was a partial heart transplant using valves from a donor heart, but her ventricular function was deteriorating so quickly that they couldn’t afford to wait weeks for one to become available.
Mia’s valves, meanwhile, functioned completely normally, and they were the right size for Brooklyn’s heart. “The timing was actually very serendipitous,” says Dr. Goldstone, who is also assistant professor of surgery in the section of Pediatric and Congenital Cardiac Surgery at Columbia University Vagelos College of Physicians and Surgeons. “We had wanted to do a valve transplant for another patient before, but we were never able to get a suitable donor in the timeframe that we needed. We all thought doing this as a domino was a great idea, and everyone came together amazingly to coordinate this incredible, life-saving procedure.”
Not only would the valve transplant — a procedure that’s been done only a handful of times before and never as part of a domino procedure in infants — save Brooklyn’s life, but a successful surgery also would be groundbreaking for other children with valve disease.
“This procedure is truly disruptive. Because the valves from Mia’s heart are living valves, they have the potential to grow and self-repair with Brooklyn,” says Dr. Kalfa, who is also associate professor of surgery in the section of Pediatric and Congenital Cardiac Surgery at Columbia University Vagelos College of Physicians and Surgeons. “None of the other options have growth potential, and all would need to be replaced multiple times with open-heart surgery before adulthood. We knew the procedure would transform Brooklyn’s quality of life.”
A History-Making Night
After the team realized they were ready to do the domino transplant, both families were immediately notified. The Skaatses were in the NCICU and had already received the joyous news that a donor heart was available. When they were told that Mia could be a donor too, they didn’t hesitate to pay it forward.
“We know what it’s like to wait and worry about your child day in and day out,” says Mia’s mom, Nicole Skaats. “We’re grateful that not only is Mia a recipient of a beautiful gift, but that she also had the opportunity to be a donor, and that hopefully that gift would help improve another child’s life.”
For the Civil family, the decision posed more uncertainty. They were at home and weren’t prepared to hear that Brooklyn would have to come in that day to receive the lifesaving surgery. “When we got the call, at first we were a little overwhelmed, but we had our parents on the call to be an extra set of ears to help us make the decision,” says Brooklyn’s mom, Sam Civil. “After talking to the team, we realized this was by far the best situation for her.”
“We were a little skeptical at first because it was something that’s never been done before,” Brooklyn’s dad, Andre Civil, adds. “But all the doctors did a good job of giving us all the information and allowed us to make an executive decision. We made the right one.”
Brooklyn arrived at the hospital later that morning so she could undergo testing first to ensure that her coronary arteries were healthy enough for surgery. Around 5 p.m., with Mia’s donor heart on the way, Dr. Goldstone and Mia and Dr. Kalfa and Brooklyn entered operating rooms across the hall from each other to start preparing the girls to receive their transplants.
Mia’s donor heart arrived around 9 p.m. Dr. Goldstone led a seven-person surgical team, including Dr. Emile Bacha, chief of the Division of Cardiothoracic Surgery at NewYork-Presbyterian Morgan Stanley Children’s Hospital, to remove her heart, which was then immediately transported to Dr. Kalfa’s operating room. Dr. Bacha then went across the hall to assist Dr. Kalfa’s team.
As Dr. Goldstone and his team continued with Mia’s heart transplant, Dr. Kalfa, who led a nine-person surgical team for Brooklyn, and Dr. Bacha began dissecting the aortic and pulmonary roots (which include the valves and the vessels they live in) from Mia’s old heart.

Dr. Kalfa transplanted the aortic root into Brooklyn’s heart to replace her leaky truncal valve. Because Brooklyn didn’t have a pulmonary valve, Dr. Kalfa also had to reconstruct parts of the right side of her heart so he could transplant the pulmonary valve where it should have been. Dr. Goldstone finished Mia’s heart transplant around 3 a.m., and then headed across the hall to assist Dr. Kalfa and his team with the remainder of Brooklyn’s surgery. By 5 a.m., Brooklyn’s valve transplant was done; her heart now had a normal anatomy.
The whole team had made history — but mainly, they had given two girls the promise of a normal, healthy future.
“When I went to see Brooklyn’s parents, the whole family was there crying, and actually I cried as well. That was really a meaningful moment in my life,” says Dr. Kalfa. “Bottom line, it was all about compassionate care, teamwork, excellence, and innovation.”
“Being a part of something like this completely rejuvenates you and reinforced to me why I became a doctor,” adds Dr. Goldstone. “It’s an operation I will remember for the rest of my life.”
Thankful for a New Normal
Mia and Brooklyn both recovered well and were discharged within a day of each other about two weeks post-surgery. “Mia has very few, if any, limitations on her lifestyle moving forward. We’ll continue to see her because she does require continuous medical care, but she should have a full, healthy life,” says Dr. Richmond, who is also associate professor of pediatrics in the Department of Pediatric Cardiology at Columbia University Vagelos College of Physicians and Surgeons. “And both of Brooklyn’s valves are functioning beautifully. We expect her to recover and thrive and grow and do all the normal things that we would want her to do at 3 months old.”
And normal is exactly what the girls’ parents want for them. “We just want to have Mia experience the simple things she missed out on, like going for walks outside or seeing our friends and family at the beach,” says Nicole. “We were here for seven months, and all the staff made the holidays, the weekends, and even the tough times the best they could be while she was living in the hospital.”
“It’s been a long journey,” adds Mia’s dad, James Skaats. “We’re so grateful to everyone for all that they did to get us to this point.”
Brooklyn’s parents already see big changes in her. “She’s constantly cooing and talking to people, she’s very smiley, and she’s starting to grab for things,” says Sam. “My hope for Brooklyn is just having a normal, happy life, with a lot fewer surgeries and procedures.”
Adds Andre, “From the surgeons all the way to the people who restock the equipment that the nurses need, everyone’s been fantastic. We can’t say anything more highly of everybody.”
Before the baby girls’ discharge day, the two sets of parents decided to come together in the playroom to meet the families who had helped change their daughters’ lives — after all, there was no way of knowing if their paths would cross again.
“We have a lot in common,” says Andre. “Meeting them was everything.”
For the staff, seeing the girls leave is bittersweet, but ultimately, it’s the result the team worked so hard for. “Seeing how grateful the families are really just motivates us to continue to push the envelope, continue to offer these newer techniques,” says Dr. Richmond. “To be able to make a difference in the lives of patients is a gift. It’s why we’re here.”

