Gastroesophageal Reflux
Gastroesophageal reflux disease (GERD), also called acid reflux, is a common digestive disorder in which stomach contents regurgitate (reflux) into the esophagus. Also called heartburn, GERD often causes inflammation and damage to the esophagus and occasionally to the lungs and vocal cords. Prolonged untreated GERD can lead to Barrett’s esophagus, a dangerous precancerous condition.
Signs & Symptoms
Patients with GERD may suffer from a wide spectrum of symptoms including heartburn, regurgitation and dysphagia (difficulty swallowing).
Causes
GERD has a variety of causes. Abnormality or weakness in the LES (lower esophageal sphincter — a muscle at the junction of the esophagus and stomach), usually associated with hiatal hernia, contributes to the failure of the body's natural anti-reflux mechanism.
Diagnosis
It is important that the diagnosis and particular cause of the GERD be confirmed. The patient's history of signs and symptoms is reviewed, and tests are performed including:
- Manometry
- pH probe
- An upper endoscopy may also be necessary to look for possible areas of stricture. Biopsies (small tissue samples) can also be obtained from an endoscopy to confirm the diagnosis of esophageal inflammation and to exclude Barrett's esophagus, the transformation of esophageal cells into stomach lining cells after years of reflux.
- Other tests include an upper GI series or a barium swallow x-ray, which can show the acid reflux and inflammation of the esophagus as well as the presence of hiatal hernia, which occurs when the upper part of the stomach moves up into the chest through a small opening in the diaphragm, often causing LES dysfunction.
Treatments
Medical therapy, consisting of anti-acid medications and lifestyle modifications, results in symptomatic relief for most patients. Surgical therapy is indicated for patients in whom medicine has proven ineffective, is poorly tolerated, or is too expensive to continue. It is also indicated for complications of reflux disease such as an esophageal stricture (narrowing) and the development of pre-cancerous changes in the esophagus.
For those patients in whom a medical regimen has not been successful, anti-reflux surgery can offer gratifying, durable results with relief of GERD. While GERD can have several causes, surgery is most effective for those patients whose GERD is caused by a defective lower esophageal sphincter (LES), the muscle connecting the esophagus with the stomach.
Both surgical and endoscopic techniques are available depending upon the patient's specific case. Our gastrointestinal specialists were among the first to perform endoscopic suturing for gastroesophageal reflux and continue to evaluate its efficacy. They are actively testing new endoscopic devices. These minimally invasive procedures may enable the patient to return home the same day.
Fundoplication Surgery
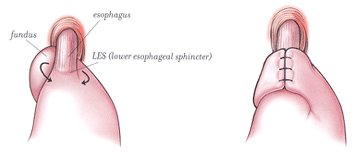 More than 90% of patients who undergo fundoplication have no reflux after surgery. The goal of the procedure is to restore the physiologic equivalent of the LES by wrapping the stomach around the lower esophagus.
More than 90% of patients who undergo fundoplication have no reflux after surgery. The goal of the procedure is to restore the physiologic equivalent of the LES by wrapping the stomach around the lower esophagus.
As the stomach becomes distended during a meal, the wrap compresses the lower esophagus, preventing reflux, thus imitating the action of a valve. Hiatal hernia, if present, may be repaired during the procedure. For patients who have other problems contributing to or accompanying their GERD, such as a swallowing disorder, a shortened esophagus, or gastric outlet obstruction, there are variations to this surgery so that there is a better overall control of symptoms.
During the operation, the surgeon raises the liver to expose the junction between the stomach and the esophagus. A space is created behind the esophagus and the fundus of the stomach and freed from its attachment to the spleen. The fundus is then pulled behind the esophagus and secured in place. Depending on the type of procedure, the wrap is either sutured to the esophagus itself, or it is sutured to the stomach on the other side of the wrap.
Endoscopic Repair of GERD
Instruments and a small camera are inserted through the mouth and advanced to the junction between the esophagus and the stomach, where the stomach is tacked alongside the esophagus in order to create a more effective barrier to reflux. The surgeon performs the procedure entirely through the mouth without making any external or internal incisions. Read more here about the totally incisionless procedure now offered at NYP/Columbia.
This procedure is ideal for patients who:
- Have a positive pH test
- Are at least partially responsive to proton pump inhibitor medicines (PPIs)
- Who have significant non-acid regurgitation
- Who prefer to be off medication
After Surgery for GERD
Most patients are able to return home the first or second day after laparoscopic surgery and 4 to 7 days after the open operation. A soft diet is recommended for several weeks after surgery.
Return to full activity usually takes 1 to 2 weeks following most laparoscopic anti-reflux repairs and 4 to 6 weeks after an open repair. For about 2 weeks after your surgery, you will need to take an acid reducing medication. A follow up appointment should be made with your surgeon 7 to 10 days after discharge so that your questions can be answered, your progress can be assessed and you can be examined.
Next Steps
If you are in need of help for an esophageal condition, we’re here for you. Call us now at (212) 305-1909 or fill out our online form to get started today.
Related Topics
- Achalasia
- Barrett's esophagus
- Esophageal atresia
- Esophageal cancer
- Esophageal dilation
- Esophagectomy
- Gastroesophageal reflux disorder (GERD)
- Hiatal hernia
- Swallowing disorders/dysphagia
