Guide to Colonoscopy
Reviewed by the physicians of Columbia’s Colorectal Surgery Team, March 2024
What is a colonoscopy?
Colonoscopy is a safe, effective method of examining the full lining of the colon and rectum. While the patient is under mild sedation or monitored anesthesia if deeper sedation is preferred, the physician inserts a flexible fiberoptic instrument called a colonoscope into the rectum and advances it through the colon (large bowel). It is used to diagnose colon and rectum problems and to perform biopsies and remove colon polyps.
Who should have a colonoscopy?
- In patients with no gastrointestinal problems and no risk factors for colon cancer, the American Cancer Society recommends a first screening colonoscopy at age 45.
- Your physician may also recommend a colonoscopy exam if you have change in bowel habit, bleeding, or other symptoms indicating a possible problem in the colon or rectum.
- If you have any risk factors for colon cancer such as Crohn's disease, ulcerative colitis or a family history of colon cancer, your screening should begin at age 40 or at least 10 years before the age your relative was when diagnosed.
- The frequency of colonoscopy is determined based on your risk factors and whether or not you have polyps on your colonoscopy. In the average risk patient with a normal colonoscopy, the test is repeated every 5-10 years.
How should I prepare for colonoscopy?
- The colon must be completely clean for the procedure to be accurate and complete. This is done one to two days before the exam with an oral solution prescribed by your physician.
- Colonoscopy is generally conducted on an outpatient basis in our endoscopy suite.
- You will receive instructions from your doctor's office regarding the time your test is scheduled and what time you should arrive at the hospital.
- Since you will receive intravenous sedation for the procedure, please have a family member or a friend meet you at the hospital after your test to assist you in returning home.
How is colonoscopy performed?
- While you are in a comfortable position on your side or on your back, the colonoscope is inserted into the rectum and advanced to the portion of the colon where the small intestine joins the colon.
- As the colonoscope is withdrawn, the lining is carefully examined. Your physician will remove polyps or take biopsies as necessary.
- The procedure usually takes about 20 minutes to perform.
- There is often a feeling of pressure, bloating, or cramping at times during the procedure, which is related to the air that is put in the colon during the exam. The doctor gives you intravenous sedation to help you relax and tolerate any discomfort during the procedure.
- Colonoscopy is usually well tolerated with minimal discomfort. Following the colonoscopy, there may be slight discomfort which quickly improves with the expelling of gas.
What are the benefits of colonoscopy?
- Colonoscopy is the most accurate way to inspect the colon to detect polyps or early cancer.
- With colonoscopy, it is now possible to detect and remove most polyps without abdominal surgery.
- Removing polyps is an important step is the prevention of cancer.
What are the risks of colonoscopy?
- Colonoscopy is a very safe procedure with complications occurring in less than 1% of patients.
- These risks include bleeding, a tear in the intestine (perforation), risk of anesthesia and failure to detect a polyp.
What are polyps and how are they removed?
- Polyps are abnormal growths from the lining of the colon which vary in size from a tiny dot to several inches.
- The majority of polyps are benign, but it can be difficult to discern whether a polyp is benign or cancerous by its outer appearance alone. Therefore, polyps are removed and analyzed microscopically.
- Removal of colon polyps is an important means of preventing colon cancer as the majority of cancers develop from polyps.
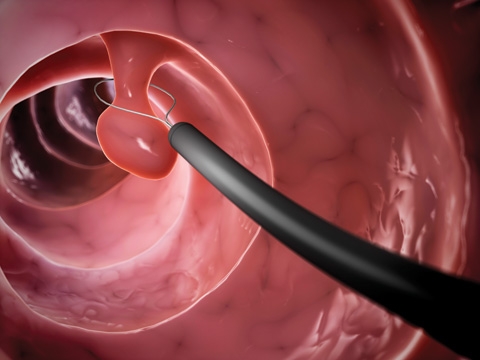
- Tiny polyps may be completely destroyed by biopsy. Larger polyps are removed by a technique called snare polypectomy, in which a wire loop is passed through the colonoscope and the polyps are cut from the intestinal wall by means of a small electrical current.
What can I expect after the colonoscopy?
After the test, you will be monitored in the recovery room until most of the effects of the medication have worn off. You may feel some cramping or bloating because of the air introduced into the colon during the examination. This should disappear quickly with the passage of gas.
- Diet: Generally, you should be able to eat normally after the colonoscopy. If your doctor recommends diet modifications, you will be instructed regarding this. If you feel nauseous or are having persistent pain, you should inform the recovery room nurse or call your doctor. If you feel the onset of nausea when you start to eat, it is best to stop eating; usually the nausea will pass and you will be able to resume eating several hours later. Sometimes this nausea or upset stomach is due to the medications given during the colonoscopy.
- Biopsy Results: It will take about one week to receive the results of your biopsy. If you have not received the results from your doctor's office after 1 week, contact your physician.
- Activity: You should not drive a vehicle or perform strenuous activities on the afternoon or evening following colonoscopy. Unless you have had a polypectomy, you should be able to resume all normal activities the day after your colonoscopy. If you have any doubts about resuming an activity, call your doctor.
- Medications: You should resume your usual medications on the evening following your colonoscopy. It is especially important that you resume taking your cardiac and blood pressure medications. However, if you have diabetes and are taking insulin, do not resume your full insulin dose until you are tolerating a regular diet. If you have any questions regarding your insulin dosage, please call your internist or general practitioner. Unless prescribed by a physician, avoid aspirin, Motrin®, Advil® or similar analgesics for 2 to 3 days. In general, when you resume your diet you should also resume your prescribed medications. For other blood thinners such as Plavix® and Coumadin®, your physician should give you specific instructions.
Things to Watch Out For
Colonoscopy is generally a very safe procedure. However, in rare circumstances, complications can occur. If you develop any of the symptoms below, call your doctor.
- Abdominal Pain: a small amount of abdominal discomfort following the test is normal. If you have a small amount of stomach upset, 1 tablespoon of Mylanta® or Maalox® may be very helpful. However, if you have persistent abdominal pain, or find that your abdominal discomfort is getting worse either the day of the test or several days thereafter, it is important that you contact your doctor.
- Bleeding: A small amount of rectal bleeding after the colonoscopy is normal. However, if rectal bleeding is severe and persistent, contact your doctor.
- Fever: If you develop a fever above 100.4 in the 2 to 3 days following your colonoscopy.
Please consult your surgeon to address any questions or concerns regarding your diagnosis or treatment.
Bowel Preparation Prior to Colonoscopy
Our standard for Bowel Preparation is Miralax but in some instances your doctor may indicate an alternate preparation.
Click here for Colonoscopy Bowel Preparation Guide.
Next Steps
If you or someone you love is in need of care for a colorectal issue, we’re here to help. Our team is available for consultations, second opinions, and to perform any colorectal procedure, should one be necessary. Call us at (212) 342-1155 or request an appointment online.
