By Elisabeth Geier
Key Takeaways:
- Advances in immunotherapy have significantly boosted survival rates for lung cancer patients, offering hope and new treatment options.
- Institutions like Columbia's immunotherapy program spearhead groundbreaking trials, including FDA-approved treatments before surgery, revolutionizing care for lung cancer patients.
- From molecular profiling to tailored therapy plans, personalized care maximizes effectiveness, and ongoing research promises even more targeted treatments.
Lung cancer is the second most common cancer in the United States, with over 200,000 cases diagnosed annually. It’s also the most deadly cancer in the United States. But over the past five years, the survival rate has increased by 14 percent. In addition to reduced smoking rates and earlier detection, advances in immunotherapy have driven that change.
At Columbia, a world-renowned immunotherapy program offers patients the newest therapies and clinical trials, altering the treatment landscape for patients living with lung cancer.
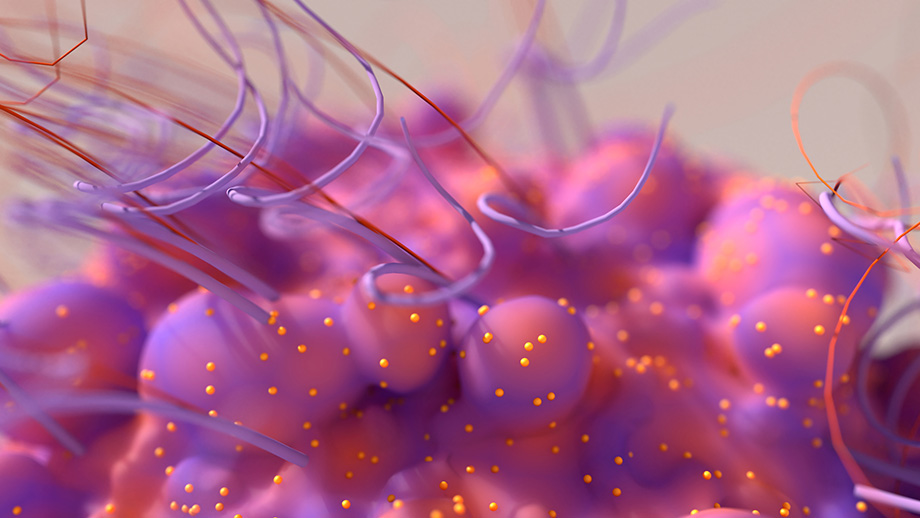
Joshua Sonett, MD, Chief of General Thoracic Surgery at NewYork-Presbyterian/Columbia, compares cancer to a stealth fighter jet: it sneaks in and evades the immune system using receptors that block the body from recognizing it. Immunotherapy is the counterattack that “basically stops this hiding,” harnessing a person’s own immune system to recognize, locate, and destroy cancer cells.
“We generally have known for years that the healthier a person is, the better their immune system works,” says Dr. Sonett. “Now, we have medicines that help to really gear it up, to help the immune system naturally attack these cancers.”
Being at the forefront of immunotherapy research for quite some time means developing and implementing many of the protocols used to treat cancer with immunotherapy. More recently, Columbia led a major pilot trial that secured FDA approval for immunotherapy lung cancer treatment before surgery. Now, all but the latest stages of lung cancer are being offered the hope for a cure.
“The results are remarkable,” says Dr. Sonett, “and what’s particularly gratifying is that it doesn't stop you from using other therapies.” Immunotherapy is typically implemented alongside treatments like chemotherapy to give patients the best chance at positive outcomes. “I like to think of it as an additive bonus to our generalized holistic care,” he says.
Most patients with lung cancer, especially non-small cell lung cancer, are candidates for immunotherapy. Patients who are not candidates can include those who have what Dr. Sonett calls “autoimmune-related diseases like myasthenia gravis or scleroderma, diseases where the patient's body is already attacking themselves.”
The decision for whether or not to use immunotherapy, and at what point in the treatment process, depends on the patient. Dr. Sonett outlines three strategies for determining how to use immunotherapy to treat lung cancer:
- Duration, or how long to continue immune therapy to help fight cancer. “Some patients are on therapies for a long time,” says Dr. Sonett.
- Combination with other treatments. Doctors consider what additive therapies, such as chemotherapy or molecular targeted personal therapy, would improve the results for immunotherapy. “We now know that chemotherapy and immunotherapy can combine very nicely together,” says Dr. Sonett. “We’re not as well-versed in how immunotherapy is needed or helps with targeted therapy.”
- Tumor composition. “Every patient that has lung cancer should have their tumor completely identified molecularly and genetically,” says Dr. Sonett. “There are a host of new genes and proteins we can target with medications that are actually better than chemotherapy, because they directly inhibit cancer growth without making the body toxic.”
Every patient that comes to NYP/Columbia for lung cancer treatment has their tumor molecularly profiled in a process called reflex testing. This information helps doctors best treat the patient in relation to their specific tumor. It’s all part of a personalized care program that structures treatment plans according to individual needs.
Immunotherapy research and development continues to make new advancements every year. Dr. Sonett is particularly excited about the potential for personalized cancer vaccine therapy, using tumor cells from a patient to create a personalized vaccine just for them.
“It’s not quite there for lung cancer yet,” says Dr. Sonett. “It’s still in research because it’s kind of expensive to do.” But at some point in the not-too-distant future, vaccine therapy will provide an additional boost to help the immune system fight against the lung cancer from which it derives. “If you put in the context of how quickly they got vaccines working for COVID, you can imagine this, the speed at which vaccine therapy for lung cancer is accelerating.”
While the COVID-19 pandemic has placed incredible strain on the medical system, one beneficial side effect is the rapid advancement of research into immunotherapy. Dr. Sonett says the general increase in research money and energy towards vaccine therapy will ultimately help save lives.
“It’s like when NASA did a moonshot: all sorts of fantastic technology got spun off,” he explains. COVID research has opened doors for additional immunotherapy research, and the results are promising. “We're learning to unlock the immune system and how to treat it with vaccines,” says Dr. Sonett, “And that will continue to improve our therapy for all cancers. We should be seeing some very exciting news in the near future.”
Related:
- New Lung Cancer Screening Guidelines Will Save Lives, But There’s Still Work To Do
- Patient successfully receives first combined COVID-19 lung transplant and triple bypass
- I Love The Skin I Am In—Life After Nuss Procedure for Chest Deformity