Guide to Radioactive Iodine
The thyroid uses iodine from the diet to make thyroid hormone and is one of the few organs that will take up iodine. Radioactive iodine (RAI) is a radioactive form of iodine that can be used to either scan or ablate (i.e. destroy) thyroid cells. Radioactive iodine has been used safely in medicine since the 1920's. The salivary glands (i.e. the glands that make saliva) take up small amounts of iodine. The RAI that is not taken up by thyroid cells is eliminated from the body, primarily in urine. Using RAI is a safe and effective way to test and treat thyroid conditions. Extensive studies have shown that patients who have been treated with small doses of radioactive iodine are not at increased risk for thyroid cancer or any other type of cancer.
RAI Scanning
 RAI is administered by mouth and images are taken to determine where in the thyroid or other parts of the body the RAI is being taken up. This testing provides information not only about the size and shape of the thyroid gland, but also about its function. In addition to I-131, technetium-99m pertechnetate or iodine-123 (other similar radioactive substances) may also be used. A minimal amount of radioactive substance is used, in order to avoid damaging the thyroid gland. Pictures of the thyroid gland are then obtained at varying time periods (hours to days) after the ingestion of these substances (either in pill or liquid form). Thyroid scanning is typically used to evaluate patients for hyperthyroidism or thyroid cancer recurrence.
RAI is administered by mouth and images are taken to determine where in the thyroid or other parts of the body the RAI is being taken up. This testing provides information not only about the size and shape of the thyroid gland, but also about its function. In addition to I-131, technetium-99m pertechnetate or iodine-123 (other similar radioactive substances) may also be used. A minimal amount of radioactive substance is used, in order to avoid damaging the thyroid gland. Pictures of the thyroid gland are then obtained at varying time periods (hours to days) after the ingestion of these substances (either in pill or liquid form). Thyroid scanning is typically used to evaluate patients for hyperthyroidism or thyroid cancer recurrence.
Hyperthyroidism
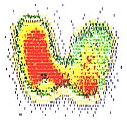
 Hyperthyroidism is a disease in which all or parts of the thyroid are overactive and making too much thyroid hormone. See Hyperthyroidism ». RAI scanning can help determine if the entire gland is hyperactive (usually seen in Graves' disease) or if only specific nodules are hyperactive (i.e. toxic adenoma). If the RAI is taken up by the thyroid more than normal, then the thyroid is considered to be "hot" or overactive. If the RAI is not well absorbed, then the thyroid is called "cold" or underactive. In the scan pictured above, the red areas are "hot," showing that this is a hyperactive thyroid gland.
Hyperthyroidism is a disease in which all or parts of the thyroid are overactive and making too much thyroid hormone. See Hyperthyroidism ». RAI scanning can help determine if the entire gland is hyperactive (usually seen in Graves' disease) or if only specific nodules are hyperactive (i.e. toxic adenoma). If the RAI is taken up by the thyroid more than normal, then the thyroid is considered to be "hot" or overactive. If the RAI is not well absorbed, then the thyroid is called "cold" or underactive. In the scan pictured above, the red areas are "hot," showing that this is a hyperactive thyroid gland.
Thyroid Cancer Recurrence
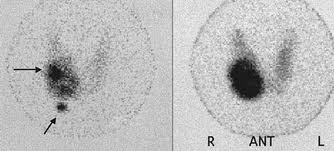
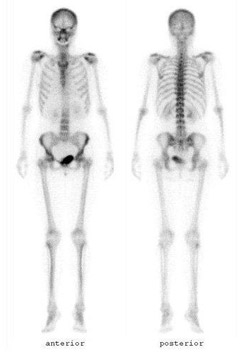 Patients who have had a total thyroidectomy for thyroid cancer may be sent for RAI scanning with potential ablation. The goal of the scan is to see if there is any remaining normal thyroid tissue (i.e. remnant) or metastatic disease. Even with a total thyroidectomy by an expert surgeon, there is usually a small remnant of thyroid tissue left behind. If patients meet certain criteria, they may be given a larger dose to destroy (i.e. ablate) the remaining thyroid tissue. During their follow-up, if the thyroglobulin level rises, an RAI scan may be ordered looking for recurrent disease. If there is recurrent or metastatic disease, a larger dose of RAI may be given to ablate them.
Patients who have had a total thyroidectomy for thyroid cancer may be sent for RAI scanning with potential ablation. The goal of the scan is to see if there is any remaining normal thyroid tissue (i.e. remnant) or metastatic disease. Even with a total thyroidectomy by an expert surgeon, there is usually a small remnant of thyroid tissue left behind. If patients meet certain criteria, they may be given a larger dose to destroy (i.e. ablate) the remaining thyroid tissue. During their follow-up, if the thyroglobulin level rises, an RAI scan may be ordered looking for recurrent disease. If there is recurrent or metastatic disease, a larger dose of RAI may be given to ablate them.
 Of note, radioactive iodine (RAI) scans used to be performed routinely for patients with thyroid nodules because "hot" (i.e. hyperactive nodules) were rarely cancer (less than 1%) while "cold" (i.e. underactive nodules) carried a 10% risk of cancer. However, FNAB is far more accurate for determining the risk of cancer and RAI scans are mostly only used in cases of hyperthyroidism.
Of note, radioactive iodine (RAI) scans used to be performed routinely for patients with thyroid nodules because "hot" (i.e. hyperactive nodules) were rarely cancer (less than 1%) while "cold" (i.e. underactive nodules) carried a 10% risk of cancer. However, FNAB is far more accurate for determining the risk of cancer and RAI scans are mostly only used in cases of hyperthyroidism.
RAI Ablation
In addition to scanning for thyroid tissue, RAI can be used to ablate (i.e. destroy) thyroid cells. The two main reasons for RAI ablation are hyperthyroidism and treatment for thyroid cancer.
Hyperthyroidism
RAI ablation cures hyperthyroidism by destroying the hyperactive thyroid cells. The goal of RAI ablation for hyperthyroidism is to destroy the thyroid and make the patient hypothyroid (i.e. no functioning thyroid tissue). For this reason, patients will require thyroid hormone replacement pills. A single dose of RAI is typically given in pill form. Occasionally, 10%, a second dose of radioactive iodine is needed. Only a few percent of people fail this second dose and require surgery to remove the overactive thyroid gland. RAI ablation takes several months in order to have its full effect, although symptoms usually improve after about four weeks. Additional anti-thyroid medications and beta-blockers may be necessary to control hyperthyroidism during this initial time period.
Thyroid Cancer
After total thyroidectomy for cancer, if patients meet certain criteria, they may be given a dose of RAI to destroy (i.e. ablate) the remaining thyroid tissue. This treatment is usually done 6 to 8 weeks after the thyroidectomy. In addition, during their follow-up, if the thyroglobulin level rises, an RAI scan may be ordered looking for recurrent disease. If there is recurrent or metastatic disease, a larger dose of RAI may be given to ablate them. Depending on the amount needed to destroy the cells, you may need to be hospitalized to monitor you and reduce the risk of radiation exposure to family and friends. Typically, only one dose of RAI ablation is needed. It is critical to consult with a thyroid specialist who can help determine the need, ideal dose, and safe administration of RAI for thyroid cancer.
Preparation for RAI Ablation
Before the RAI therapy, the goal is to prepare the body to take up as much of the iodine as possible. This preparation is done one of two ways:
Thyroid hormone withdrawal:
The patient stops taking thyroid hormone replacement pills for four to six weeks before the treatment. Since there is no thyroid hormone in the body, the brain makes high levels of TSH which "tells" any remaining thyroid tissue to take up iodine to make thyroid hormone. Since the patient is not taking thyroid hormone replacement, they will become hypothyroid and often feel very tired and fatigued by the end of the withdrawal period. Often, they will be given Cytomel which is a short-acting form of thyroid hormone up until 2 weeks before the RAI therapy in order to minimize the amount of time they are hypothyroid. The TSH level should be at least 30 before RAI is given.
Thyrogen stimulation:
Thyrogen is a man-made form of thyroid stimulating hormone that is given as an injection on the 2 days before the RAI therapy. This therapy does not require that the patient become hypothyroid.
Both techniques appear to be equally effective. It is important to discuss with a thyroid specialist which form of preparation is best for the individual patient. In addition, patients should be on a low iodine diet for 2 weeks before the RAI therapy. Information about the low iodine diet can be found at: http://thyca.org/rai.htm#diet
Radiation Safety:
The RAI is removed from the body in the sweat, saliva, and urine. For this reason, patients who are not being hospitalized for the therapy should prepare for the following precautions they will need to follow in the first 5 days after the therapy:
- Avoid close contact (< 3 feet) with young children, elderly, and pregnant women
- Avoid sharing a toilet or bathroom. Flush with the lid down.
- Avoid sharing food.
- Avoid sharing a bed.
- Avoid kissing and sexual activity.
- Wash clothes, towels, and linens separately.
- Wash hands and the rest of the body often.
Your physician can arrange a consultation with Columbia Thyroid Center radiation safety specialists both prior to your ablation and during treatment. They will discuss your specific needs during the treatment.
Side Effects of RAI Ablation
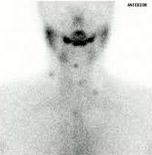
Short-term side effects of RAI therapy may include nausea and vomiting soon after treatment, which usually lasts a day or two. In addition, some of the RAI may be picked up by the salivary glands around the jaws and under the tongue, causing painful swelling and enlargement of these glands. This is treated by drinking plenty of fluids, sucking on lemon drops (in order to stimulate the flow of saliva), and occasionally pain medicine such as aspirin or acetaminophen.
It is important to note, that pregnant or breast feeding woman should never receive RAI for any reason because it may destroy the developing fetus' thyroid. Patients should wait 6 to 12 months after RAI before attempting to get pregnant. Although RAI can pose a risk to your baby's thyroid, radioactive iodine itself does not cause infertility or other birth defects.
Next Steps
If you are dealing with a thyroid issue, our team at the Columbia Thyroid Center is here to help. Call (212) 305-0444 or request an appointment online.
Related Conditions
- Graves’ Disease
- Hyperthyroidism
- Hypothyroidism
- Multinodular Goiter
- Thyroiditis
- Thyroid Nodules
- Thyroid Cancer: Overview | Types | Causes | Symptoms | Diagnosis | Treatment | Prognosis/Outcomes
- Papillary Thyroid Cancer
- Follicular Thyroid Cancer/ Hurthle Cell Carcinoma
- Medullary Thyroid Cancer
- Anaplastic Thyroid Cancer
- Thyroid Lymphoma
